Progress in the regional TB response reversed by the COVID-19 pandemic
The Western Pacific Region has achieved substantial advancements in tuberculosis (TB) care and prevention, resulting in a reduction of TB deaths by 42% and incidence by about 17% compared to levels in 2000. Despite these achievements, TB remains a major public health concern in the Western Pacific. In 2021, the Region saw an estimated 1.9 million people fall ill with TB and 126 900 related deaths. This is a 6.5% increase in incidence and a 38% increase in deaths compared to the previous year. This is due to significant shortfalls in TB case notifications reported in the Region for both 2020 and 2021. In 2021, approximately 1.1 million people with a new or relapse episode of TB were notified and reported to national TB programmes, down 20% from 1.4 million in 2019. The increase in people falling ill with TB and dying from TB in 2021 highlights the severe impact the COVID-19 pandemic has had on the TB response. Years of progress to end TB has been reversed.
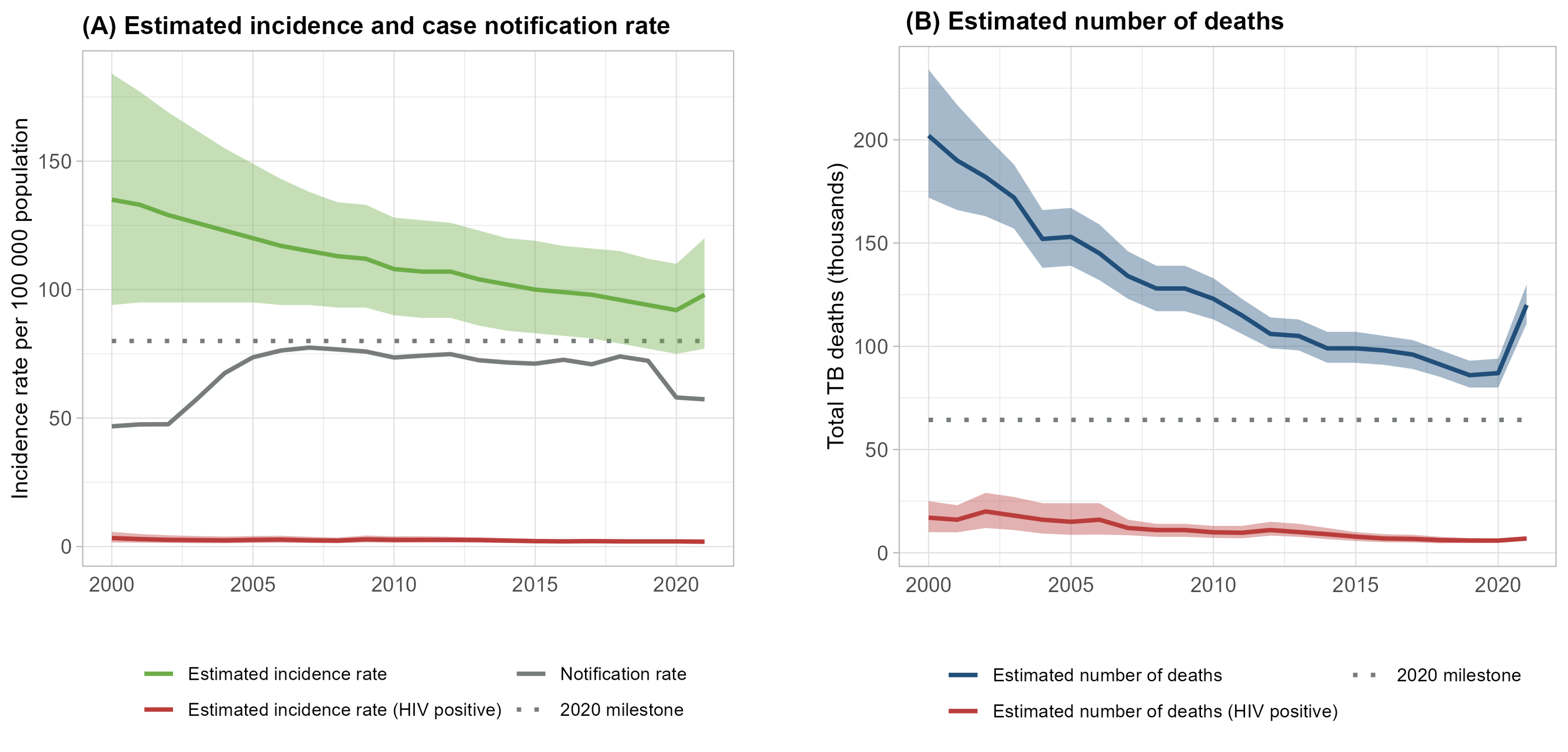
Figure 1: (A) Estimated incidence rate, case notification rate, and 2020 End TB Strategy milestone and (B) estimated number of deaths in the Western Pacific Region, 2000-2021
Limited reach of TB service: Only 63% of people with TB access TB care
The cascade of care is a framework for evaluating patient retention across sequential stages of care required to achieve a successful treatment outcome. In 2020, of the estimated 1.8 million patients in the Region, 63% were notified and 56% were successfully treated. These detection and treatment gaps were larger among multi-drug resistant/rifampicin-resistant TB (MDR/RR-TB) patients and TB/HIV co-infected patients. Of the 73,000 estimated MDR/RR-TB patients, 42% were laboratory confirmed, 33% were enrolled in treatment and 20% were successfully treated. Among TB/HIV co-infected patients, of the estimated 38,000 patients, 35% were notified and 26% were successfully treated.
Accelerated efforts are required to minimize the gaps in the care cascade. Ensuring universal and equitable access to TB services is critical to reducing the gap in case detection. Strengthening national surveillance and notification systems with the enforcement for notification, including those treated outside the public sector, is crucial to minimize under-reporting and notification. Promoting people-centered care, including community-based treatment, is essential to improve treatment adherence and minimize the gap in treatment.
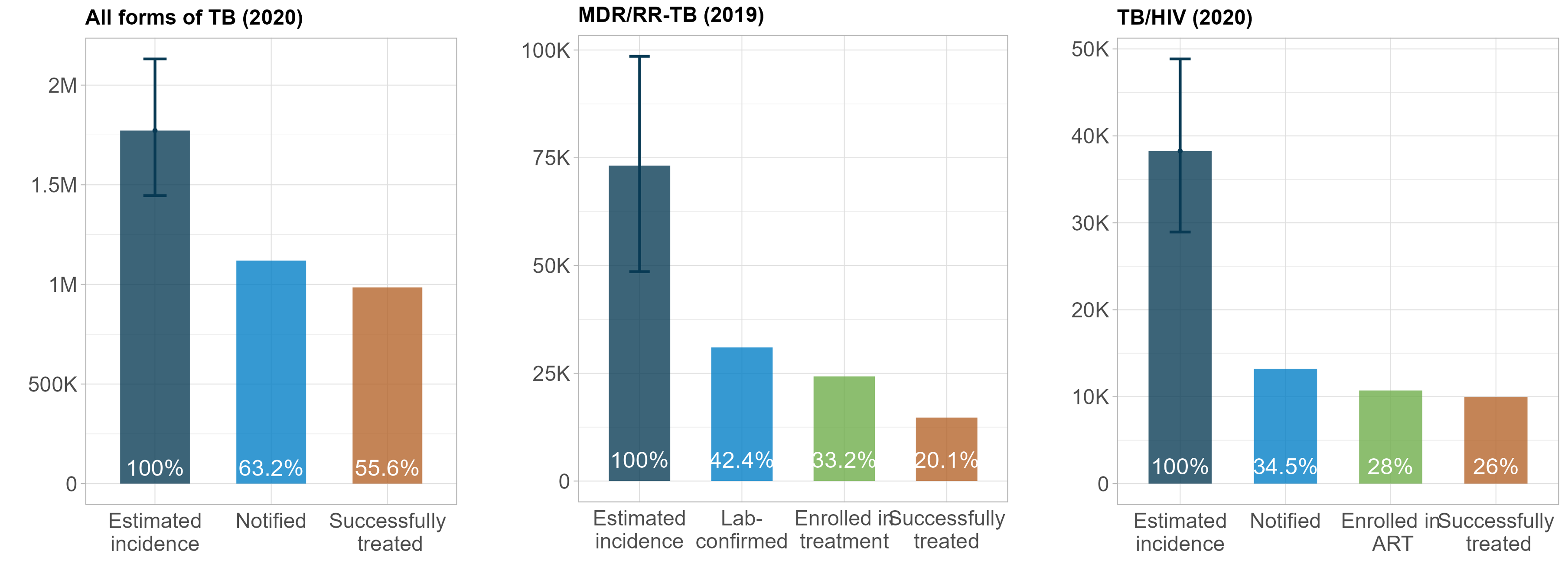
Figure 2: TB care cascade in all forms of TB, MDR/RR-TB, TB/HIV co-infected patients in the Western Pacific Region, 2019-2020
TB patients and families struggle with financial hardship
The World Health Organization (WHO) End TB Strategy includes the target that no tuberculosis (TB) patients or their households face catastrophic costs (including direct medical expenditures, non-medical expenditures and income losses) because of TB disease. Catastrophic costs are defined as the total direct and indirect costs that reach or exceed 20% of the TB patient or household’s annual expenditure or income. As of 2022, substantial proportions (34-92%) of TB-affected families were reported to have faced catastrophic costs due to TB in the eight countries in the Region that carried out national cost surveys for people with TB. Although TB care is free in many governmental health systems in the Region, considerable number of TB patients and their families suffer financial hardship. The key TB services are included within national health insurance schemes in some countries, but the percentage of population, the coverage of TB services and the proportion of costs covered by health insurance are insufficient.
Results from the national surveys showed that catastrophic costs are mainly caused by non-medical costs and income loss due to TB; poor households get poorer and people with TB lose their jobs; and the financial burden of TB is more significant among people with drug-resistant TB (DR-TB) and TB co-infected with HIV. In order to eliminate catastrophic costs due to TB, the expansion of social protection mechanisms and adequate coverage among the poor is crucial.
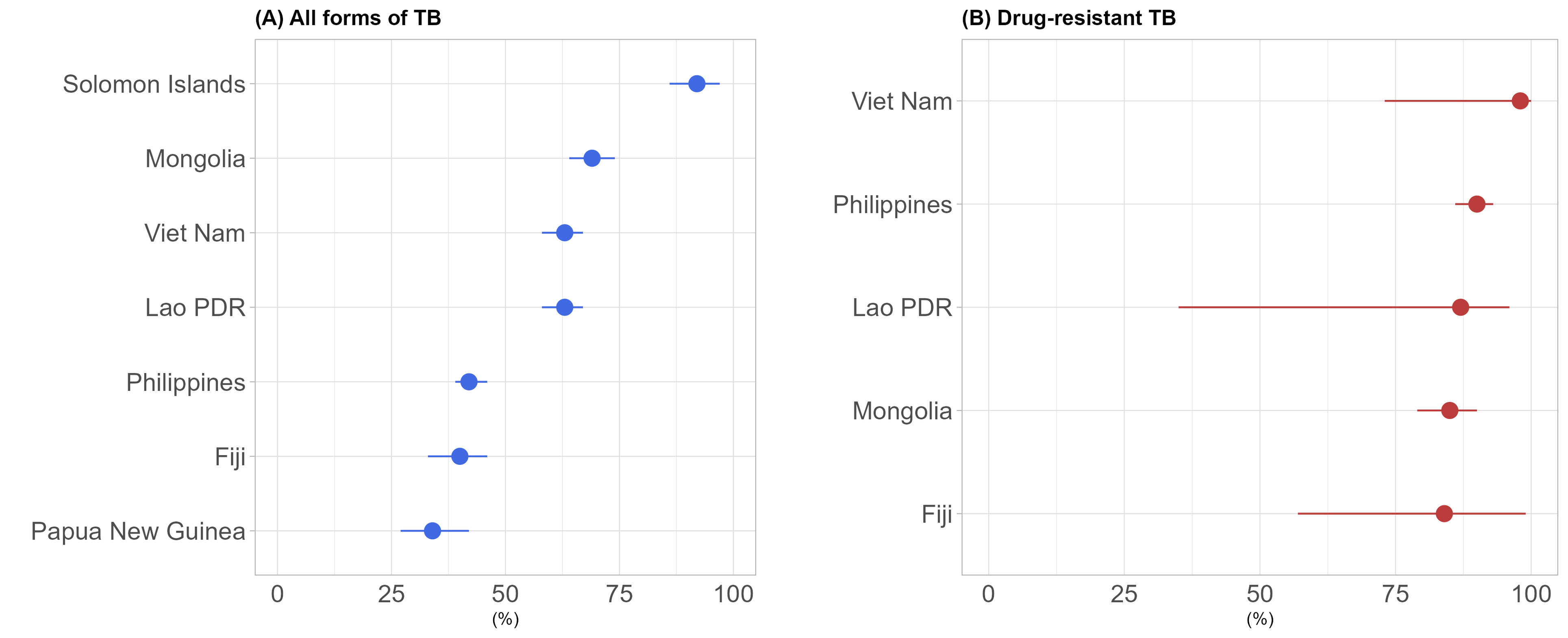
Figure 3: Estimates of the percentage of TB patients and their households facing catastrophic costs among (A) all forms of TB, and (B) drug-resistant TB
TB preventive therapy scaled up, but more efforts needed
TB preventive therapy (TPT) is a major tool for TB prevention, in addition to the early detection and treatment of active TB. Currently available TPT can reduce the risk of TB disease by 60-90%, which means that expansion of TPT would translate into major reductions in mortality and morbidity for people at the highest risk of TB. In addition, by preventing TB disease, TPT protects individuals and their families against catastrophic costs.
In the WPR, the total number of people who started on TPT increased more than 2 times in 2019 (n=63,804) compared to 2018 (n=30,246). This is mainly due to a substantial increase in the number of people living with HIV who started on TPT, from 12,112 in 2018 to 38,758 persons in 2019, and an expansion of the eligibility of TPT from child contacts <5 years old to contacts of all ages, resulted in an increase among contacts aged 5 and over from 6,075 in 2018 to 13,814 persons in 2019.
However, further expansion of contact investigation and TPT is needed considering only 40% of eligible people living with HIV and less than 10% of estimated eligible children aged 5 years and under were on treatment in 2021. Furthermore, the number of people who started on TPT was far below the target set by the UN High-Level Meeting on TB. Of the regional target of 2,255,900 people on TPT for 2018-2021, only 10% (n=236,655) were enrolled on TPT during this period, calling for further efforts to scale up. Tools such as shorter TPT regimens, digital radiography equipped with computer-aided detection software for TB and tests for TB infection to better target TPT may help to scale up TPT.
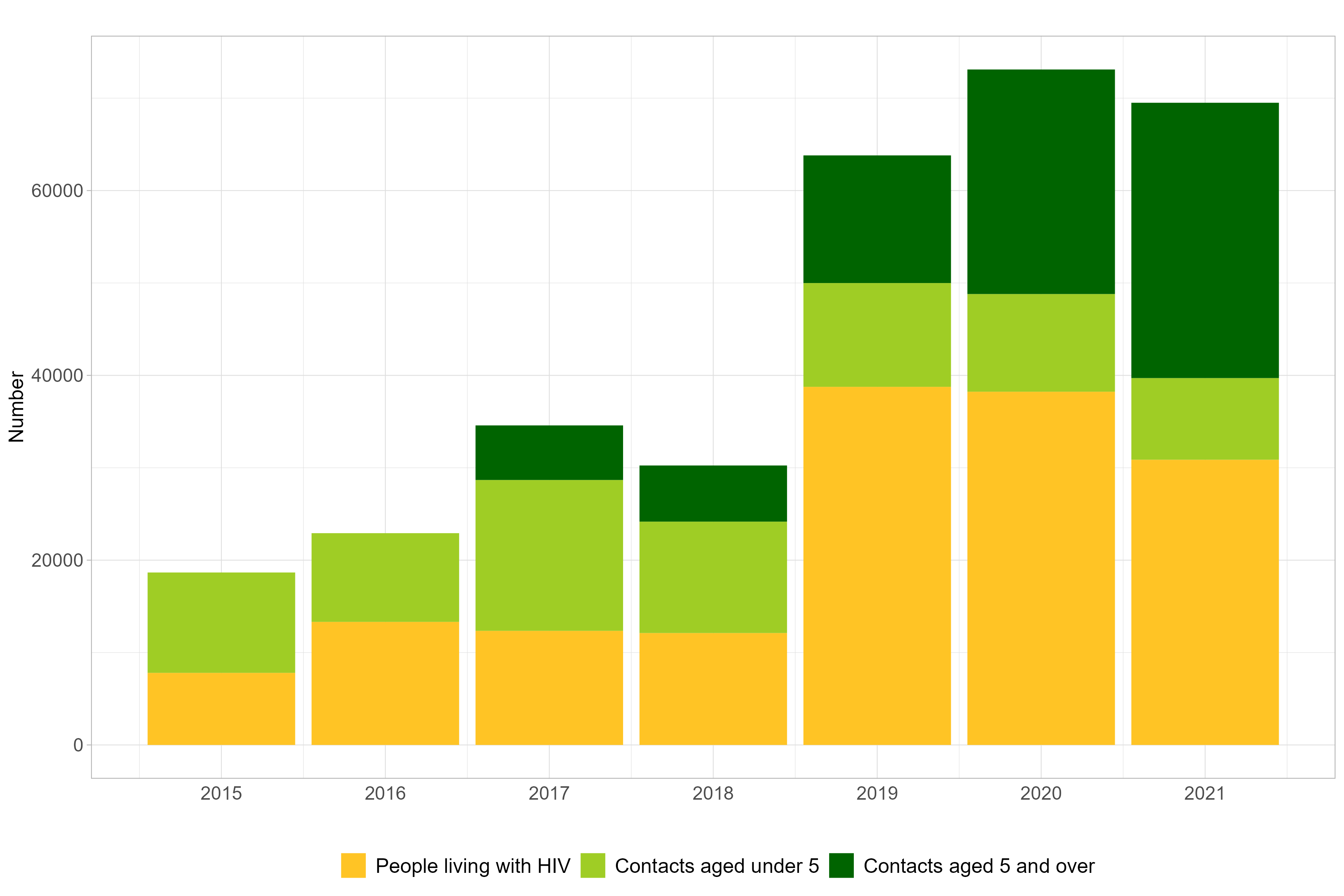
Figure 4: Number of people started on TB preventive treatment, 2015-2021
References:- TB profile 2021. World Health Organization
- Global tuberculosis report. World Health Organization
- Western Pacific Regional Framework To End TB: 2021-2030 (who.int)